Tracking down tuberculosis


Mireille Kamariza is working on an affordable test for tuberculosis.Credit: Faranak Emami/Samueli School of Engineering, UCLA
Growing up in Burundi, a country of 13 million people in East Africa, Mireille Kamariza was familiar with the devastating effects of tuberculosis (TB). “It’s a long and torturous disease,” she says. “You have relatives and loved ones that are sick, and you see them suffer through it. It’s not a quick death.”
Part of Nature Outlook: Medical diagnostics
When she moved to the United States at 17, she was struck by how different the situation was there. “The question that I had when I arrived here was, how come this is not a problem here?” That question led Kamariza, now a chemical biologist at the University of California, Los Angeles, on a quest to find ways to eradicate the disease in areas where it is widespread. A key challenge is determining who is infected, so that they can be treated and the disease stopped from spreading. But current diagnostic methods are slow, often expensive, sometimes difficult to administer and not easily accessible in the low-income regions where TB is most prevalent.
TB researchers are pushing to develop faster, more accurate and more accessible tests. In 2014, the World Health Organization (WHO) set the goal of reducing the number of new cases worldwide by 80% between 2015 and 2030; it considers widespread screening and rapid diagnosis as crucial to achieving this. Replacing older testing methods with newer diagnostic and screening techniques could help individuals with the disease to be identified quicker and start treatment before their symptoms worsen — potentially before they can spread the disease. “It’s the people who have TB and don’t know they have it, they’re the ones who are spreading the disease,” says Jerry Cangelosi, an environmental-health scientist at the University of Washington School of Public Health in Seattle.
TB has been infecting people for at least 9,000 years, and it has often been the leading cause of infectious-disease deaths globally. It was eclipsed in the past few years by COVID-19, but, as the pandemic wanes, TB could retake the top spot. According to the WHO, an estimated 10.6 million people caught TB globally in 2022 and 1.3 million died1.
The disease is caused by Mycobacterium tuberculosis, a microorganism that is spread through coughing, sneezing and spitting. It thrives in crowded conditions where there is poverty, poor nutrition and a lack of accessible health care. Fortunately, the disease is treatable with antibiotics, and the drugs used now are less toxic and taken for a shorter time than those used in the past — a few months, rather than a couple of years — even for drug-resistant strains. Around 4% of new cases are resistant to multiple drugs, and that rises to 19% among people who have previously received treatment.
But treatment and prevention require the identification of people who have and could spread the disease. “There’s a huge gap in the number of TB cases that we know are out there and what we’re actually diagnosing,” says Adithya Cattamanchi, a pulmonologist and epidemiologist at the University of California, Irvine. At least 3 million people of the WHO’s 10.6 million estimate are undiagnosed, he says.
Part of the problem, Cattamanchi says, is that the most prevalent test for TB is the sputum smear test, for which health-care workers collect a mix of saliva and mucus coughed up from the lungs; stain it with auramine, a dye that attaches to a large family of bacteria; and examine it under a microscope. The technique behind the test was developed in the 1880s by the German microbiologist and Nobel prizewinner Robert Koch. “It’s still, 150 years later, the test that we most commonly use,” Cattamanchi says.
But it has limitations. Some people have trouble coughing up sputum; people with HIV and children under five are less likely to produce much of the substance. Health-care workers collecting the sample could be exposed to the pathogen while the person is coughing. The thick sputum has to be thinned to be placed on a microscope slide. Finding the bacteria can take a day or two, and even then, it is unknown whether the strain is drug resistant. To work this out, physicians can culture the bacteria against various drugs — but that takes several weeks, which can delay administration of the right treatment. Often, physicians simply start people on the most common treatment and see whether they improve.
Molecular tests can be faster than microscopy and more accurate than cultures, because they can amplify DNA and identify resistant strains directly. But the uptake of such tests has been slow. Nucleic acid amplification tests (NAATs) have been available for almost three decades, but the earliest ones were labour intensive and required specialized skills to administer. More recent NAATs, such as the semi-automated polymerase chain reaction tests, can identify the bacteria and whether they are resistant to the first-choice antibiotic, rifampicin, in about three hours. These tests still have limitations, Cattamanchi says, because the equipment is expensive and needs to be kept in a facility that can reliably supply power and maintain an appropriate temperature — putting the machines out of reach of many local health-care facilities, where people usually seek care first. The WHO recommended a molecular test, branded Xpert, in 2010, but the cost of the individual test cartridges is prohibitive to the communities that need them. Danaher in Washington DC, the company that sells Xpert, announced last September that it was lowering the price from US$10 per cartridge to $8. But health advocates want that to go down to $5, which they say would make the test more accessible while still allowing the company to make a profit.
Bodily fluids
Kamariza is working on a cheaper diagnostic test, a fluorescent tag that binds to a product of living TB bacteria and makes them quickly identifiable under a microscope. Although fluorescent probes are common in biology, there are surprisingly few for TB, she says. In fact, auramine is the only other one.
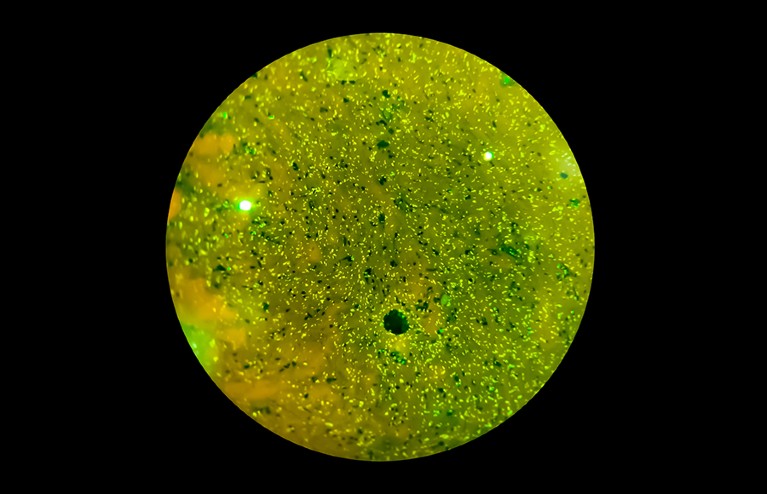
The microorganism Mycobacterium tuberculosis causes tuberculosis and is spread through coughing and sneezing.Credit: Bani Khatun/Getty
Kamariza developed a dye molecule that binds to a sugar, trehalose, on the surface of the bacterial cell. Staining a sputum sample with the dye does not require much preparation, Kamariza says, and the bacteria light up in minutes. While still a PhD student at Harvard University in Cambridge, Massachusetts, she co-founded a company — OliLux Biosciences, based in Los Angeles — to commercialize the probe. Since then, she has learnt that although her dye was easy to spot with the high-end microscope in her laboratory, it was too dim for the cheaper equipment used in a typical clinic in Uganda, where the company is testing the assay. So she is developing a brighter dye that those microscopes can detect1.
For now, Kamariza’s method still requires sputum and a microscope. That could change, however; she has collected some data (not yet published) suggesting that it will work on bacteria in blood samples as well. Although this is not the molecular approach that the WHO is pushing for, Kamariza feels that her test could be an intermediate step — many countries do not have the infrastructure to use molecular tests widely. She hopes that her test can speed up the identification of resistant strains during culturing as well. Getting results in a day or two will lead to people receiving the correct treatment more quickly, she says.
Other researchers are looking beyond sputum. Biochemist Tony Hu, who directs the Center for Cellular and Molecular Diagnostics at Tulane University’s School of Medicine in New Orleans, Louisiana, is developing several tests to detect products of TB bacteria in blood samples, which could be collected by a finger prick. In one test, he introduces a nanoparticle engineered to bind to a particular protein produced by the bacteria, called CFP-10. The nanoparticle amplifies the protein in the sample, making it more detectable by a mass spectrometer. Hu tested the method on blood samples from children under five, who can be difficult to diagnose because their TB symptoms can be attributable to other diseases. He found TB in 100% of children who also had HIV and had had TB confirmed by another method, and in 84% of children with HIV who had tested negative with other methods but were later diagnosed2. People with HIV are more likely to have extrapulmonary TB, which leaves fewer bacteria in the lungs and makes it harder to diagnose.
Hu also uses nanoparticles to target the TB-associated proteins lipoarabinomannan (LAM) and lipoprotein LprG. Cells shed waste by releasing particles called extracellular vesicles, which, in people with TB, contain LAM and LprG. “The most important thing for us is the abundance,” Hu says. “One cell can secrete 10,000 vesicles every day.” And those vesicles persist in the blood for longer than the proteins alone would, making them available for detection.
Hu coats his nanoparticles with antibodies that bind to the vesicles, and then looks for them using a microscope3. He’s even designed and tested a small system that can replace the microscope. It includes a smartphone and an objective lens, and uses a mobile app — aided by a machine-learning algorithm that screens out background noise — to find the nanoparticles. The portable device showed results similar to those from a microscope. A third test that Hu has developed, which uses gene-editing technology to amplify TB DNA floating in the blood, is also simple. It uses a paper strip to hold the sample, a small amount of reagent and a smartphone-sized reader4.
Another easy-to-collect sample is urine, which also contains LAM. The first WHO-recommended version of a LAM urine test has low sensitivity, identifying only about 40% of people with TB if they are also infected with HIV, and 20% of people without HIV5. New generation urine tests are being developed that have a sensitivity of around 70%.
That’s not as high as physicians would like, but the tests are still useful for targeted populations, such as people with HIV, says Ruvandhi Nathavitharana, an infectious-disease specialist at Harvard Medical School in Boston, Massachusetts. “If you can do a urine-based bedside test and it’s positive, then a clinician can get that person on TB treatment straight away,” she says.
Algorithm-aided screening
Whereas urine collection requires some privacy, swabbing people’s tongues is so straightforward that a nurse could walk around a classroom testing students while they sat at their desks, says Cangelosi. That sort of community screening will be necessary to get TB under control, he says. And “if we want to envision going into workplaces or schools or communities and actively screening people, sputum collection is a non-starter”.
Even when it’s not easy for someone to produce sputum, TB bacteria come up from the lungs when people cough, and land on the back of the tongue, where they can persist for hours6. So far, tongue swabs have not proved as sensitive as other tests, but that could be because they’re being used in conjunction with testing platforms that have been optimized for sputum, Cangelosi says. That could change, however. The COVID-19 pandemic led many diagnostic companies to develop platforms for testing nasal swabs, and those could be adapted for tongue swabs.
Whether it involves tongue swabs or another approach, community screening is important to stem the spread of TB. Chest X-ray has a venerable history as a screening tool. “We used it way back when in the United States to really reduce the prevalence of TB,” Cattamanchi says. Today’s portable, digital X-ray machines don’t require the expensive film and process of past machines, and they can be placed in local health centres or driven around in a van. The main barrier to X-ray screening is a lack of skilled radiologists to interpret the scans.
To address that shortage, several research groups are using artificial intelligence (AI) to identify TB in lung images. Google, for instance, has been training an AI system using X-rays of people who are known to have TB, so that the tool can learn how the various types of lung damage caused by the disease look in an image and can spot them in new X-rays7. People flagged by the AI tool could then take a more established type of test, such as a NAAT, to confirm whether they have TB, says Daniel Tse, a health researcher at Google Research in Mountain View, California. Such screening, which Google’s test7 found was comparable with that performed by radiologists, could reach more people and mean that diagnostic tests are targeted more specifically, keeping costs down. For now, Tse says, images are processed by Google’s cloud servers, but for areas that have unreliable Internet access, the diagnostic algorithm might be stored on a smartphone or a dongle. Google has licensed the technology to Right to Care, a non-profit health-care organization in Centurion, South Africa.
AI could be applied to other information as well. Researchers at Stellenbosch University in South Africa, for instance, are working on algorithms that can identify TB from coughing sounds, recorded by a smartphone8. Others have explored doing something similar with lung sounds recorded by digital stethoscopes9. Tse says that several researchers are exploring whether an AI tool that combines multiple data sources might boost TB identification further.
Screening and diagnostic tests are continuing to improve, but to really fulfil their potential, they need the kind of funding and political will that was directed against the COVID-19 pandemic, says Nathavitharana. “The technologies are advancing, but honestly, it’s too slow,” she says. “We saw how much could be achieved for COVID in a very short time with the resources and targeted attention.” TB is both preventable and curable, and a major push could end its devastation, she argues. “No one should be dying of a disease like TB when we can do better.”






